“The Evolution of Gestation Length in Mammals”
 Dr. Antonis Rokas | Rokas Lab
Dr. Antonis Rokas | Rokas Lab
Bio:
Antonis Rokas is a professor at the Departments of Biological Sciences and of Biomedical Informatics at Vanderbilt University and a holder of the Cornelius Vanderbilt Chair in Biological Sciences. He also serves as the founding director of the Vanderbilt Evolutionary Studies Initiative (http://www.vanderbilt.edu/evolution), an interdisciplinary center that unites scholars from diverse disciplines with broad interests and expertise in evolution-related fields. Rokas received his B.S. in Biology from the University of Crete, Greece (1998) and his Ph.D. from Edinburgh University, Scotland (2001). Before joining Vanderbilt in the summer of 2007, he was a postdoctoral fellow at the University of Wisconsin-Madison (2002–2005) and a research scientist at the Broad Institute (2005–2007). Research in the Rokas lab focuses on the study of the DNA record to gain insight into the patterns and processes of evolution. Through a combination of computational and experimental approaches, his current research aims to understand the molecular foundations of the fungal lifestyle, the reconstruction of the tree of life and the evolution of human pregnancy-associated traits.
Abstract:
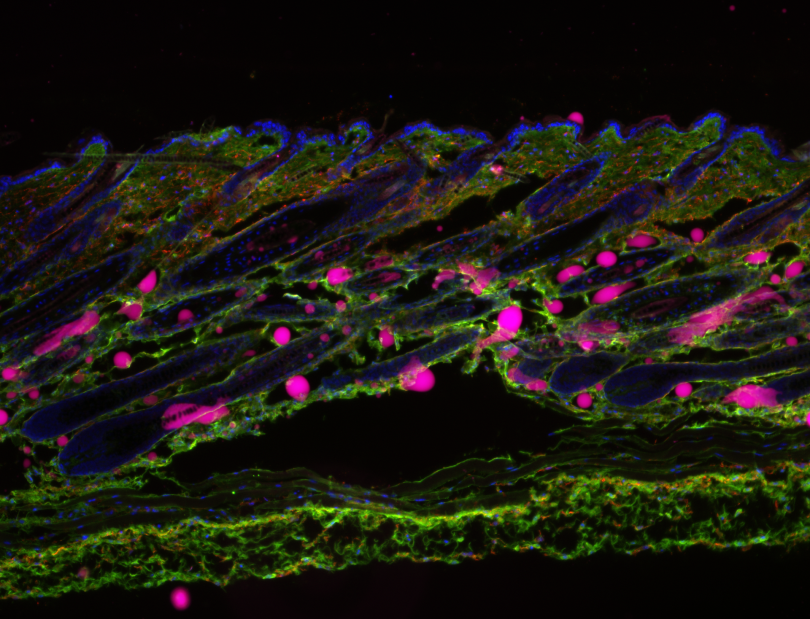
Eutherian mammals have characteristic lengths of gestation that are key for reproductive success, but relatively little is known about the processes that determine the timing of parturition. This issue remains one of biology's great unsolved mysteries and has significant clinical relevance because preterm birth is the leading cause of infant and under 5-year-old child mortality worldwide. In my talk, I will describe my team’s and collaborative efforts to understand the genetic architecture of gestation length in (European) humans, the evolutionary forces acting on human loci involved (and an approach for extending this for any complex trait), and the evolution of gestation length in relation to other life history traits across mammals.

 Dr. Yvon Woappi
Dr. Yvon Woappi